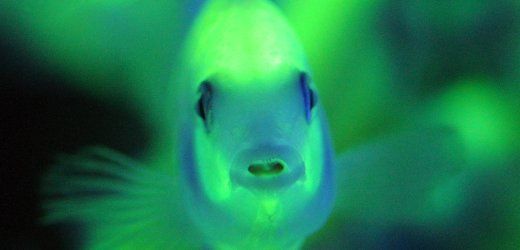
[dropcap style=”font-size:100px; color:#992211;”]U[/dropcap]CSF scientists use tiny zebrafish to screen for drugs to help control obesity, diabetes, and other conditions.
A tiny, translucent zebrafish that glows green when its liver makes glucose has helped an international team of researchers identify a compound that regulates whole-body metabolism and appears to protect obese mice from signs of metabolic disorders.
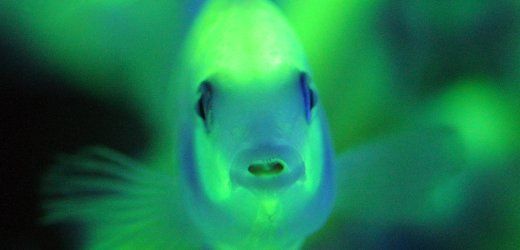
Led by scientists at the University of California, San Francisco (UCSF), the work demonstrates how a fish smaller than a grain of rice can help screen for drugs to help control obesity, type 2 diabetes and other metabolic disorders, which affect a rising 34 percent of American adults and are major risk factors for cardiovascular disease.
Described this week in the journal Nature Chemical Biology, the new compound emerged from a panel of 2,400 medications and drug-like compounds tested in the zebrafish. The test was designed to identify key regulators of “fasting metabolism”— a state most people face every day after the lingering remnants of their long-digested meals pass slowly down their digestive tract.
Fasting metabolism is the body’s way of fulfilling its energy needs between meals by turning to fat and other stored sources. It involves a carefully balanced and coordinated cascade of reactions that see numerous genes in various tissues kick into action and do things like burn fat.
In type 2 diabetes and other metabolic diseases, this careful balance is lost.
“The body cannot keep up with the breakdown of energy, and lipids [molecules of fat] can accumulate to toxic levels in the liver,” said UCSF postdoctoral fellow Philipp Gut, MD, who led the research with Didier Y.R. Stainier, PhD, a professor in the Department of Biochemistry and Biophysics.
How the Screen Works
Some screens can be conducted in cell culture by taking living cells grown in the laboratory and exposing them to various drugs. The ability to rapidly test large libraries of compounds in the last few decades through such screens has revolutionized biomedical science.
But looking for drugs that regulate biological processes like metabolism, which involves multiple interacting organs in the body, and even more types of cells, cannot be done in cell screens because they lack the same complexity. Mice are often used to test pharmacological compounds, but screens of this magnitude would require thousands of mice, which would be ethically impossible to justify and prohibitively expensive.
Gut and his colleagues set out to develop the zebrafish screen as an ethical and inexpensive solution, and the new paper demonstrates the validity of this approach, he said. Furthermore, this study illustrates the fact that model organisms should be an integral part of the new roadmap defined by the NIH and other medical research organizations around the world to translate the most advanced laboratory science into benefits for patients, Stainier said.
Of the thousands of compounds the team screened, two appeared to turn on a handful of genes that caused the animals to burn fat as a way of producing energy – an end that would be desirable for many people with metabolic disorders.
Further experiments with one of these compounds in mice showed that it could protect obese mice from metabolic problems.
(Study information)
The article, “Whole-organism screening for gluconeogenesis identifies activators of fasting metabolism,” by Philipp Gut, Bernat Baeza-Raja, Olov Andersson, Laura Hasenkamp, Joseph Hsiao, Daniel Hesselson, Katerina Akassoglou, Eric Verdin, Matthew D Hirschey and Didier Y R Stainier will be published online by the journal Nature Chemical Biology on Dec. 2, 2012.
This study was supported by the National Institutes of Health through grant #P30 DK026743, #P30 DK063720, #DK59637, #NS051470, #U01 DK089541 and #RO1 DK60322 and by a grant from the American Heart Association. Additional funds were provided by the Gladstone Institutes, the Glenn Foundation for Medical Research and through a postdoctoral fellowship from the German Research Foundation.
In addition to UCSF, authors on this study are associated with the Gladstone Institutes in San Francisco; Duke University Medical Center in Durham, N.C.; Karolinska Institutet in Stockholm, Sweden; the Garvan Institute of Medical Research in New South Wales, Australia; and the Max Planck Institute for Heart and Lung Research in Bad Nauheim, Germany.
UCSF is a leading university dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. (Source Eurekalert)
The aim of art is to represent not the outward appearance of things, but their inward significance. – Aristotle